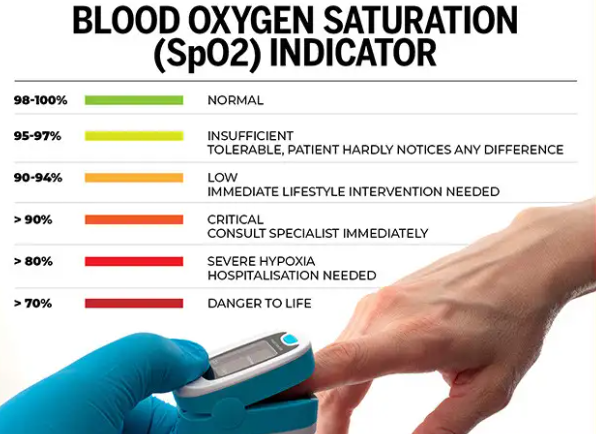
Understanding dangerously low oxygen levels is crucial for recognizing when immediate medical attention is needed. Oxygen saturation measures the percentage of oxygen in your blood, with normal levels ranging from 95% to 100%. A dangerously low oxygen level usually refers to a blood oxygen saturation below 90%, with levels at or below 88% deemed critical, often requiring urgent care to prevent organ damage, especially to the brain and heart.
What Does a Dangerously Low Oxygen Level Mean?
A dangerously low oxygen level, medically termed hypoxemia, indicates insufficient oxygen in the blood to meet the body’s needs. This condition can rapidly affect vital organs, causing symptoms such as confusion, rapid heartbeat, shortness of breath, cyanosis (bluish skin or lips), dizziness, and fatigue. If oxygen levels fall below 85%, immediate emergency intervention is critical because prolonged hypoxia (low oxygen in tissues) can lead to coma, seizures, or death.
How Is Oxygen Level Measured?
Oxygen levels are most commonly measured using a pulse oximeter, a non-invasive device clipped on a fingertip that estimates blood oxygen saturation (SpO2) and pulse rate. Normal SpO2 is typically 95% or higher. Regular monitoring is essential for individuals with lung or heart conditions, especially when symptoms of low oxygen appear. Arterial blood gas (ABG) tests provide more detailed oxygen content and blood chemistry but require a blood draw.
Common Symptoms and Signs of Low Oxygen
Early signs of dangerously low oxygen levels include lightheadedness, confusion, rapid or shallow breathing, increased heart rate, fatigue, and cyanosis. As oxygen levels drop further, coordination and judgment may decline, followed by fainting, loss of consciousness, and severe neurological impairment. Recognizing these symptoms early can prompt timely intervention and prevent permanent damage.
Causes of Dangerously Low Oxygen Levels
Various conditions can cause low oxygen levels, including chronic respiratory diseases (COPD, asthma), infections like pneumonia or COVID-19, heart conditions, high altitudes, and sleep-related breathing disorders such as sleep apnea. Certain medications or substances that depress breathing (opioids, alcohol) can also lower oxygen saturation during sleep or rest.
Treatment and Management
Immediate treatment focuses on increasing oxygen intake, often via supplemental oxygen delivered through nasal cannulas or masks. In emergency settings, mechanical ventilation may be needed. Long-term management includes addressing underlying causes—using inhalers, antibiotics, pulmonary hygiene, or lifestyle adjustments—and careful monitoring of oxygen levels. Advanced AI-powered devices now help provide real-time insights for patients with chronic conditions.
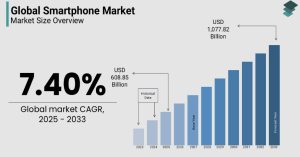
Comparative Overview of Oxygen Saturation Levels
| Oxygen Saturation (SpO2) | Significance | Symptoms and Effects |
|---|---|---|
| 95% – 100% | Normal blood oxygen level | Healthy oxygenation |
| 90% – 94% | Mild hypoxemia | Possible fatigue, mild breathlessness |
| 88% – 90% | Dangerously low, critical threshold | Immediate risk; requires medical evaluation |
| Below 88% | Severe hypoxemia, life-threatening | Cyanosis, confusion, rapid heartbeat, loss of consciousness |
Who Should Be Concerned?
People with chronic pulmonary or cardiac diseases, elderly individuals, those living in high-altitude regions, or patients recovering from respiratory infections should monitor oxygen levels closely. Sleep apnea sufferers and athletes training at altitude may also benefit from oxygen monitoring to prevent hypoxia-related complications.
Scenario Applications
-
Commercial: Workers in confined spaces should maintain oxygen above 19.5% to avoid cognitive impairment and physical weakness.
-
Sleep: Sleep-related hypoxemia is common in obstructive sleep apnea; oxygen levels dropping below 88% during sleep require intervention.
-
Exercise: Athletes training at altitude must watch oxygen saturation to avoid fatigue and performance decline.
-
Outdoor: High-altitude climbers risk hypoxia; portable pulse oximeters aid in early detection of dangerously low levels.
Recommended Actions If Oxygen Levels Are Low
If pulse oximetry shows oxygen saturation below 90%, seek emergency medical help immediately. Sit upright to improve airflow, avoid exertion, and if available, use supplemental oxygen until professional care is accessed.
Related Brands and Devices for Monitoring
-
Wrist-worn pulse oximeters by Fitbit and Garmin
-
Standalone fingertip pulse oximeters like those from Nonin and Zacurate
-
Clinical-grade ABG tests in healthcare settings
Comparison Table: Popular Pulse Oximeters
| Brand | Measurement Accuracy | Battery Life | Connectivity | Price Range | Unique Feature |
|---|---|---|---|---|---|
| Nonin Onyx Vantage | ±2% SpO2 | 20 hours | None | High | Clinical-grade FDA approved device |
| Zacurate Pro Series | ±2% SpO2 | 30 hours | None | Affordable | Portable with quick reading |
| Fitbit Sense | ±2-3% SpO2 | 6+ days | Bluetooth | Mid-range | Integrated health ecosystem |
| Garmin Venu 2 | ±2% SpO2 | Up to 11 days | Bluetooth | High | Fitness tracking with SpO2 measures |
FAQ
Q: What blood oxygen level is considered dangerously low?
A: Blood oxygen saturation below 90% is generally considered dangerously low and requires prompt medical evaluation.
Q: Can low oxygen levels be asymptomatic?
A: Yes, mild hypoxemia may cause no symptoms until it worsens, making monitoring important for at-risk individuals.
Q: How can I increase my blood oxygen level quickly?
A: Sitting upright, deep breathing exercises, fresh air, and supplemental oxygen can help raise levels quickly in mild cases.
Q: Are pulse oximeters reliable?
A: Pulse oximeters are generally accurate but can be affected by cold fingers, nail polish, or poor circulation.
Q: When should I seek emergency care for low oxygen?
A: If SpO2 falls below 90% or symptoms like confusion, severe shortness of breath, or cyanosis occur, seek emergency care immediately.