
The year 2025 marks a pivotal moment in the transformation of medical imaging. AI is now a driving force behind faster and more precise diagnoses, helping healthcare professionals identify diseases with remarkable accuracy. This shift is supported by significant market growth: the global AI-based medical image analysis industry is projected to reach unprecedented levels, with a compound annual growth rate (CAGR) expected to soar through the decade. These advancements not only enhance diagnostic capabilities but also address critical challenges, such as the increasing demand for efficient healthcare delivery.
Key Takeaways
-
AI helps find problems in medical images that people might miss.
-
AI makes reading scans faster, helping doctors decide quickly and work better.
-
AI tools do boring tasks for radiologists, so they can handle harder cases and help patients more.
-
AI makes blurry images clearer, helping doctors give accurate results even with bad scans.
-
AI predicts treatments for each patient, making them healthier and avoiding extra procedures.
The Role of AI in Medical Imaging
Enhancing Diagnostic Accuracy
Artificial intelligence is transforming how you approach diagnostic accuracy in medical imaging. AI tools analyze complex medical images with precision, helping you identify abnormalities that might be missed by the human eye. For example, a study from Harvard Medical School highlights how AI systems interact with radiologists differently. While some radiologists see improved performance with AI assistance, others may experience challenges. This shows the importance of tailoring AI models to individual needs for maximum benefit.
AI’s ability to enhance diagnostic accuracy is evident in real-world applications. At Stanford University, an AI system outperformed human radiologists in detecting pneumonia from chest X-rays. Similarly, AI-assisted mammography screenings at Massachusetts General Hospital reduced false positives by 30%, maintaining high sensitivity for breast cancer detection. These advancements demonstrate how AI tools can improve outcomes and reduce errors in medical image analysis.
Moreover, AI algorithms excel in tasks like image segmentation. They delineate structures in medical images with remarkable accuracy, aiding in treatment planning and surgical precision. Whether it’s early disease detection or personalized medicine, AI empowers you to make informed decisions that improve patient care.
|
Study Focus |
Key Findings |
|---|---|
|
Early Disease Detection |
AI systems analyze medical images quickly and accurately for timely interventions. |
|
Image Segmentation |
AI enhances treatment planning by accurately identifying structures of interest. |
|
Personalized Medicine |
AI generates patient-specific insights, enabling tailored treatment plans. |
|
Image-Guided Interventions |
AI improves surgical outcomes with augmented visualization and navigation. |
Reducing Scan-Read Times
AI tools are revolutionizing how quickly you can interpret medical images. By automating routine tasks, AI reduces the time needed to analyze scans, allowing you to focus on more complex cases. For instance, computer-assisted detection tools prioritize scans in emergency departments, speeding up the diagnostic process.
Quantitative studies highlight the impact of AI on scan-read times. A German study on worklist prioritization reduced reading times from 80 minutes to 35-50 minutes. Similarly, an algorithm for detecting intracranial hemorrhages cut reading times from 16 minutes to 12 minutes. These reductions streamline your workflow, enabling faster clinical decisions.
|
Study/Method |
Reduction in Reading Time |
|---|---|
|
CAD for normal cases |
Decreased reading time |
|
Vessel suppression on CT |
21% reduction |
|
Worklist prioritization |
Reduced from 80 min to 35-50 min |
|
Intracranial hemorrhage detection |
Reduced from 16 min to 12 min |
AI-powered solutions also improve report turnaround times. In some cases, these times have dropped from 11.2 days to as low as 2.7 days. This acceleration ensures that patients receive timely diagnoses and treatments, enhancing overall healthcare efficiency.
AI for Radiology: Supporting Radiologists with Advanced Tools
AI for radiology is not about replacing you but empowering you with advanced tools. These tools act as intelligent assistants, automating repetitive tasks and flagging abnormalities for review. This allows you to dedicate more time to complex cases that require your expertise.
AI systems trained on extensive datasets enhance both diagnostic accuracy and efficiency. For example, they help you interpret X-rays and CT scans with greater precision. In emergency settings, AI tools prioritize critical cases, ensuring that you can address urgent needs promptly.
Radiology workflows also benefit from AI’s ability to integrate seamlessly with existing systems. By automating routine processes, AI reduces your workload and minimizes burnout. It acts as a reliable partner, enabling you to deliver better patient care while maintaining high productivity.
Tip: Think of AI as an ally in your practice. It’s designed to complement your skills, not replace them. By leveraging AI tools, you can improve clinical precision and focus on what matters most—your patients.
Applications of AI in Medical Image Analysis
Image Reconstruction for Better Clarity
AI has revolutionized image reconstruction, enabling you to achieve clearer and more detailed medical images. Advanced AI techniques, such as convolutional neural networks (CNNs) and generative adversarial networks (GANs), significantly enhance image quality. These methods reduce noise and improve resolution, ensuring that you can make accurate diagnoses even with low-quality or incomplete scans.
For instance, CNNs reduce noise by up to 50%, maintaining diagnostic accuracy while improving clarity. GANs achieve structural similarity index measure (SSIM) scores exceeding 0.90, which indicates near full-dose image quality. Super-resolution GANs (SRGANs) further enhance resolution by up to fourfold, sharpening details and improving sharpness. These advancements allow you to visualize subtle anomalies that might otherwise go unnoticed.
|
AI Technique |
Improvement Description |
Performance Metrics |
|---|---|---|
|
Convolutional Neural Networks (CNNs) |
Reduces noise by up to 50%, enhancing image clarity while maintaining diagnostic accuracy. |
Noise reduction of 50% |
|
Generative Adversarial Networks (GANs) |
Achieves SSIM scores over 0.90, indicating near full-dose image quality. |
SSIM > 0.90 |
|
Super-Resolution GANs (SRGANs) |
Enhances resolution up to fourfold, improving sharpness and detail in images. |
PSNR increase of 4–6 dB over conventional methods |
By leveraging these AI tools, you can ensure that medical imaging provides the clarity needed for precise diagnoses and effective treatment planning.
Computer-Assisted Detection (CADe) for Abnormalities
AI tools equipped with computer-assisted detection (CADe) capabilities are transforming how you identify abnormalities in medical images. These systems analyze scans with remarkable speed and accuracy, flagging potential issues for further review. This ensures that no critical detail is overlooked, even in high-pressure environments.
CADe systems excel in detecting a wide range of anomalies, from cerebral metastases to hemoperitoneum. A systematic review of 24 studies revealed that deep learning algorithms achieved a pooled detectability rate of 89% for identifying cerebral metastases. AutoML models for detecting hemoperitoneum in ultrasonography demonstrated sensitivity and specificity rates exceeding 94%, with an area under the receiver operating characteristic (AUROC) curve of 0.97. These metrics highlight the reliability of AI in supporting your diagnostic efforts.
|
Metric |
Description |
Application |
|---|---|---|
|
ROC |
Receiver Operating Characteristics |
Evaluates performance with both normal and abnormal scans |
|
AUROC |
Area Under the ROC Curve |
Measures overall accuracy in distinguishing between classes |
|
FROC |
Free-Response ROC |
Used when evaluating multiple lesions per scan |
|
AFROC |
Alternative FROC |
Similar to FROC but emphasizes false positives |
|
CPM |
Competition Performance Metric |
Focuses on sensitivity and management of false positives |
By integrating CADe systems into your workflow, you can enhance diagnostic accuracy and streamline the detection process, ultimately improving patient outcomes.
AI in Emergency Care for Rapid Diagnoses
In emergency care settings, time is critical. AI empowers you to make rapid and accurate diagnoses, ensuring that patients receive timely interventions. By automating data collection and synthesizing information, AI tools streamline the diagnostic process, allowing you to focus on delivering care.
AI systems provide real-time diagnostic support, enhancing your clinical decision-making accuracy. For example, they can prioritize critical cases, ensuring that life-threatening conditions are addressed immediately. Additionally, AI facilitates rapid feedback and education through quality improvement initiatives, helping you refine your diagnostic skills.
-
AI automates data collection, reducing the time needed to gather patient information.
-
Real-time diagnostic support improves decision-making accuracy in high-pressure situations.
-
Quality improvement initiatives enhance your skills and lead to better patient outcomes.
These capabilities make AI an indispensable tool in emergency care, where every second counts. By leveraging AI, you can ensure that patients receive the best possible care when they need it most.
Predictive Analytics for Personalized Treatments
Predictive analytics powered by AI is transforming how you approach personalized treatments in healthcare. By analyzing vast amounts of patient data, AI systems can predict how individuals will respond to specific therapies. This allows you to create tailored treatment plans that improve outcomes and reduce unnecessary interventions.
AI uses data from electronic health records to identify patterns in patient demographics, medical history, and treatment responses. Machine learning models analyze this information to recommend therapies that align with a patient’s unique profile. For example, if a patient has a history of adverse reactions to certain medications, AI can suggest alternatives that are more likely to be effective and safe.
-
Machine learning develops customized treatment strategies based on individual profiles.
-
AI identifies patterns in patient data, including demographics and medical history, to guide personalized care.
These capabilities enhance your ability to deliver precision medicine. In oncology, for instance, AI can predict which chemotherapy regimens will work best for a specific cancer type. This reduces trial-and-error approaches and ensures patients receive the most effective treatment from the start. Similarly, in cardiology, AI can analyze imaging data and clinical records to recommend personalized interventions for heart disease.
Predictive analytics also streamlines your workflow by automating data analysis. Instead of manually sifting through patient records, you can rely on AI to provide actionable insights. This saves time and allows you to focus on delivering high-quality care. Moreover, predictive models can flag high-risk patients, enabling early interventions that prevent complications.
Note: Predictive analytics doesn’t just improve individual care. It also helps you identify trends across patient populations, paving the way for more effective public health strategies.
By integrating predictive analytics into medical image analysis, you can unlock new possibilities in personalized medicine. AI’s ability to process complex datasets ensures that every patient receives care tailored to their specific needs, leading to better outcomes and a more efficient healthcare system.
Challenges and Limitations of AI in Medical Imaging
Addressing Data Privacy and Security
AI in medical imaging faces significant challenges in maintaining data privacy and security. Patient data often contains sensitive information, and ensuring its protection is critical. However, large datasets required for training AI algorithms are frequently inaccessible due to privacy concerns. This limits the development of robust models.
|
Key Findings |
Description |
|---|---|
|
Increasing privacy budgets can maintain performance but restrict data access. |
|
|
Data Reconstruction Risks |
Real-world risks can be mitigated without sacrificing diagnostic accuracy. |
|
Differential Privacy (DP) |
DP offers stronger privacy guarantees than traditional de-identification. |
The risks of re-identification also pose a threat. Advanced algorithms can sometimes reverse anonymization, exposing patient identities. Public-private partnerships in healthcare have occasionally failed to provide adequate privacy protections, highlighting the need for stricter oversight.
Tip: Adopting differential privacy techniques can help you balance data utility and security, ensuring compliance with regulations while maintaining diagnostic accuracy.
Overcoming Bias in AI Algorithms
Bias in AI algorithms remains a critical issue in medical imaging. Models trained on unbalanced datasets often fail to perform well across diverse patient populations. For instance, a study on melanoma prediction revealed that AI systems trained predominantly on light-skinned images performed poorly on darker skin tones. This disparity can lead to unequal healthcare outcomes.
|
Study Focus |
Key Findings |
|---|---|
|
Melanoma Prediction |
AI models showed reduced accuracy for darker skin tones, affecting outcomes. |
|
MIMIC-III Data Set |
Class imbalance caused recall rates as low as 25%, highlighting significant bias. |
To overcome this, you must ensure that training datasets represent diverse demographics. Regular audits of AI systems can also help identify and mitigate biases, improving fairness and diagnostic accuracy.
Integration with Existing Healthcare Systems
Integrating AI into existing healthcare systems presents logistical and technical challenges. Many AI solutions struggle to align with current IT infrastructures, disrupting clinical workflows. For example, commercial systems often fail to store annotations in reusable formats, limiting their utility for AI development.
|
Barrier Type |
Number of Studies |
|---|---|
|
Workforce |
35 |
|
Education/Training |
27 |
|
Workflow Integration |
23 |
|
Financial Issues |
7 |
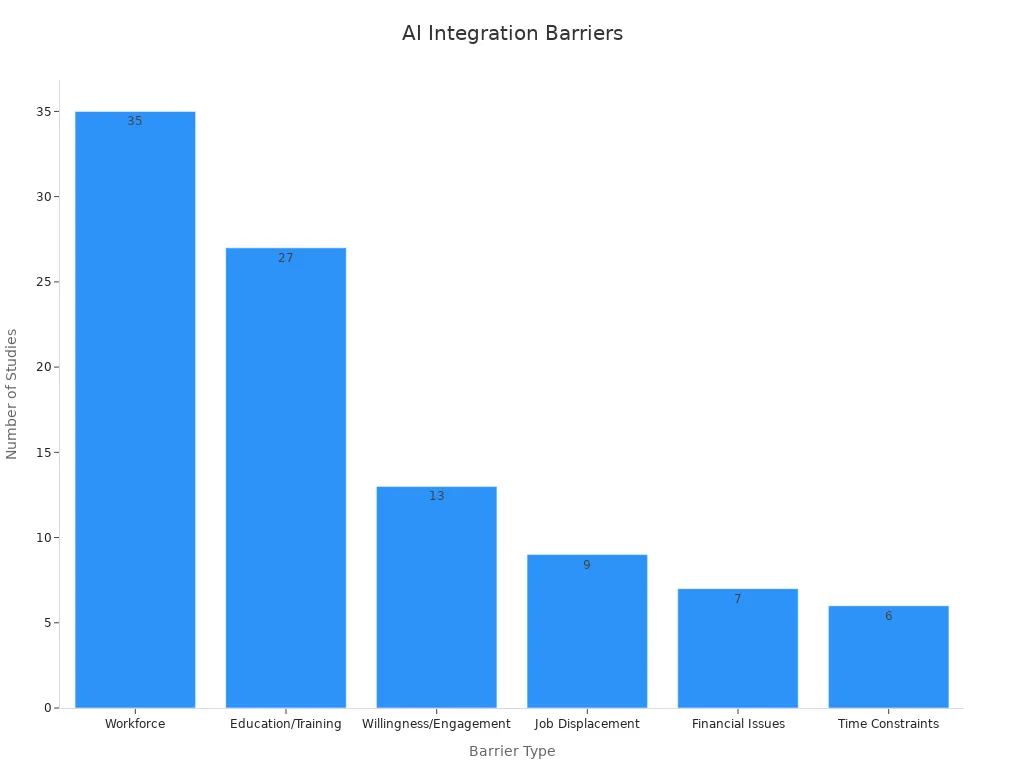
To address these issues, you should prioritize interoperability and usability when deploying AI tools. Collaborating with software engineers can ensure seamless integration, enabling radiology departments to adopt AI without disrupting their workflows.
Regulatory and Standardization Hurdles
AI in medical imaging faces significant regulatory and standardization challenges. These hurdles can slow down innovation and limit the adoption of AI tools in clinical settings. You must navigate these complexities to ensure AI systems meet safety and effectiveness standards.
One major challenge involves clinical supervision. AI-enabled devices often require oversight because they are not designed to function as standalone diagnostic tools. This means you cannot rely solely on AI for critical decisions, which adds an extra layer of responsibility. Additionally, bias in training datasets can affect how AI performs in real-world scenarios. When algorithms are trained on unbalanced data, their clinical relevance diminishes, making them less reliable for diverse patient populations.
Another issue arises from limited diversity in patient groups used during performance evaluations. This lack of representation raises concerns about whether AI tools can generalize effectively to actual clinical practice. For example, an algorithm tested only on specific demographics may fail to deliver accurate results for others. You need to ensure that AI systems undergo rigorous testing across varied populations to address this gap.
The regulatory landscape also presents obstacles. Rapid changes in documentation and evolving guidelines create uncertainty for developers. This can delay the introduction of new AI-enabled medical devices. However, organizations like the FDA are working to address this. Their updated guidance on AI and machine learning devices aims to facilitate innovation while maintaining safety standards.
|
Evidence Description |
Type of Challenge |
|---|---|
|
Clinical Supervision |
|
|
Bias in training datasets affects the real-world performance of AI algorithms, leading to concerns about their clinical relevance. |
Dataset Bias |
|
Limited diversity in patient groups used for performance evaluation raises questions about generalizability to actual clinical practice. |
Generalizability |
|
Rapid changes in regulatory documentation create barriers to innovation for developers of AI-enabled medical devices. |
Regulatory Landscape |
|
The FDA's evolving guidance on AI/ML devices aims to ensure safe and effective modifications in response to new data. |
Innovation Facilitation |
Note: To overcome these challenges, you should advocate for standardized protocols and diverse datasets. Collaboration between regulators, developers, and healthcare providers can help create a more streamlined path for AI adoption in medical imaging.
Real-World Impact of AI in Medical Image Analysis

Collaborations Between Tech and Healthcare
Collaborations between technology companies and healthcare providers are driving innovation in medical imaging. These partnerships combine cutting-edge AI tools with clinical expertise to improve patient outcomes. For example, AI systems developed by researchers like Landman aim to provide second opinions on medical images, reducing human error and enhancing diagnostic accuracy. By working together, tech and healthcare professionals ensure that AI solutions address real-world challenges in radiology and clinical decision-making.
You can see the impact of these collaborations in the development of safer imaging techniques. Research by Li and colleagues introduced an AI-enabled contrast agent that minimizes risks associated with traditional dyes. This innovation not only improves patient safety but also reduces healthcare costs, making advanced imaging accessible to more patients. These partnerships highlight how AI can transform radiology into a safer and more efficient field.
Innovations in AI Diagnostic Platforms
AI diagnostic platforms are revolutionizing how you approach clinical decision-making. Tools like VisualDx and Isabel DDx Companion assist physicians by analyzing patient data and suggesting potential diagnoses. These platforms use AI to process complex datasets, enabling faster and more accurate decision-making. For instance, Google's DeepMind algorithms predict acute kidney injury up to 48 hours in advance, allowing you to take preventive measures and improve patient outcomes.
A variety of AI tools are making diagnostics more efficient:
-
Radiology AI flags critical findings in medical images, prioritizing cases for radiologists.
-
qXR by qure.ai detects abnormalities in chest X-rays, enhancing reporting efficiency.
-
Viz.ai identifies large vessel occlusions in CT scans, facilitating rapid treatment initiation.
These innovations reduce turnaround times and improve resource allocation, ensuring that patients receive timely care. By integrating AI into your workflow, you can enhance diagnostic precision and streamline healthcare delivery.
Case Studies of Improved Patient Outcomes
Real-world case studies demonstrate how AI improves patient outcomes. At the University of Rochester Medical Center, AI implementation led to a 116% increase in ultrasound charge capture and a threefold rise in ultrasounds sent to electronic health records. Valley Medical Center saw case reviews jump from 60% to 100%, while extended observation rates improved by 25%. These results show how AI enhances efficiency and ensures better care for patients.
AI-powered tools also excel in early disease detection. Systems designed to screen for lung cancer identify the disease at earlier stages, enabling timely interventions. This approach significantly improves survival rates and reduces healthcare costs. Landman's research further highlights AI's ability to reveal hidden patterns in disease progression, offering a comprehensive understanding of patient health over time.
By adopting AI solutions, you can achieve measurable improvements in patient outcomes. These tools empower you to deliver high-quality care while optimizing clinical workflows.
The Future of AI for Radiology and Medical Imaging
Advancements in Deep Learning and Neural Networks
Deep learning and neural networks are driving the next wave of innovation in medical imaging. These advanced algorithms improve the accuracy and speed of image analysis, enabling you to detect subtle patterns in complex datasets. For instance, generative adversarial networks (GANs) now create synthetic medical images that enhance training datasets, leading to more robust diagnostic models. Additionally, integrating AI with electronic health records allows you to develop personalized treatment plans tailored to individual patient needs.
These advancements also streamline workflows. AI technology reduces interpretation delivery times for chest X-rays from 11.2 days to just 2.7 days. This efficiency not only accelerates diagnoses but also optimizes scanner usage and personnel allocation, ensuring higher-quality care. As deep learning continues to evolve, you can expect even greater precision and reliability in medical imaging.
Fully Autonomous Diagnostic Systems
Fully autonomous diagnostic systems are no longer a distant dream. Recent milestones, such as the FDA authorization of the IDx-DR system for detecting diabetic retinopathy, highlight the potential of these systems to operate without clinician oversight. This breakthrough demonstrates how autonomous AI can enhance access to specialty-level diagnostics, particularly in primary care settings.
The development timeline for these systems is promising. Pivotal trials have shown their effectiveness in real-world scenarios, paving the way for broader adoption. By incorporating autonomous systems into your practice, you can focus on complex cases while AI handles routine diagnostics with consistent accuracy.
|
Milestone |
Description |
|---|---|
|
Pivotal Trial |
Conducted for the IDx-DR system to detect diabetic retinopathy in primary care settings. |
|
FDA Authorization |
IDx-DR became the first autonomous diagnostic AI system authorized by the FDA without clinician interpretation. |
|
Implications for Primary Care |
Demonstrates the potential for autonomous AI systems to enhance access to specialty-level diagnostics. |
Expanding Access to Underserved Regions
AI has the power to bridge healthcare gaps in underserved regions. Teleradiology solutions powered by AI enable remote interpretation of imaging studies, ensuring that patients in rural areas receive timely diagnoses. These tools also prioritize urgent cases, providing preliminary findings that guide immediate interventions.
In Kenya, AI-enabled portable ultrasound devices have transformed maternal care. Midwives trained to use this technology now deliver critical care to expectant mothers in remote areas. This approach exemplifies how AI can improve healthcare equity. With approximately 80% of U.S. counties classified as healthcare deserts, AI offers a lifeline by connecting patients to essential services.
By leveraging AI, you can expand access to high-quality diagnostics, ensuring that geography no longer dictates the standard of care.
AI in Preventive Healthcare and Early Detection
AI is transforming preventive healthcare by enabling early detection of diseases and improving health outcomes. Predictive analytics powered by AI identifies high-risk patients before symptoms appear. This allows you to intervene early and prevent the progression of serious conditions. For example, AI systems analyze patient data to detect subtle patterns that traditional methods might miss. These insights help you recommend proactive measures, such as lifestyle changes or targeted screenings.
Machine learning algorithms enhance diagnostic accuracy, especially in identifying abnormalities during routine checkups. A systematic review in BMC Medical Informatics found that these algorithms outperform traditional methods in targeting high-risk patients. This means you can focus resources on individuals who need them most, optimizing both time and costs.
AI also plays a critical role in early disease detection. It scans medical images to identify potential issues, such as early-stage cancers or cardiovascular risks. For instance, AI for radiology tools can flag subtle anomalies in X-rays or MRIs, ensuring you catch diseases at their earliest stages. This improves the chances of successful treatment and reduces the burden on healthcare systems.
|
Study Title |
Findings |
Link |
|---|---|---|
|
Preventive Healthcare with AI: A Smarter Approach to Disease Prevention |
AI-driven predictive analytics improve identification of high-risk patients, leading to better health outcomes and cost optimization. |
https://lucemhealth.com/blog/preventive-healthcare-with-ai-smarter-approach-disease-prevention/ |
|
An Insight into AI and Preventative Health |
AI aids in early disease detection by identifying abnormalities and recommending proactive interventions. |
https://www.echelon.health/artificial-intelligence-preventative-health/ |
|
Systematic Review in BMC Medical Informatics |
Machine learning algorithms enhance diagnostic accuracy compared to traditional methods, allowing for targeted screening of high-risk patients. |
N/A |
By integrating AI into preventive healthcare, you can shift the focus from reactive treatments to proactive care. This approach not only saves lives but also reduces healthcare costs. AI empowers you to make informed decisions, ensuring patients receive timely and effective interventions.
AI is transforming medical image analysis in 2025, offering unparalleled benefits to healthcare systems and patient care. By leveraging advanced AI tools, you can achieve faster diagnoses, improving diagnostic accuracy and enhancing outcomes for patients. AI models now extend beyond traditional diagnostic imaging, impacting fields like pathology and genomics. These advancements enable precise disease detection and progression prediction, optimizing treatment planning and reducing healthcare costs.
The shift toward personalized medicine, powered by machine learning models, ensures tailored care for every patient. AI tools for detection streamline workflow integration, allowing you to focus on complex cases while maintaining efficiency. Since the early 2000s, AI-driven technologies have revolutionized medical imaging, empowering radiologists to deliver better care through improved diagnostic capabilities.
As AI continues to evolve, its potential to save lives and improve healthcare outcomes will only grow. By embracing these innovations, you can help shape a future where medical imaging is faster, more accurate, and accessible to all.
FAQ
What is the main benefit of using AI in medical imaging?
AI improves diagnostic accuracy and speeds up image analysis. It helps you detect abnormalities that might be missed by the human eye, ensuring faster and more reliable diagnoses. This leads to better patient outcomes and more efficient healthcare delivery.
Can AI replace radiologists in the future?
No, AI is designed to assist, not replace, radiologists. It acts as a tool to enhance your expertise by automating repetitive tasks and flagging critical findings. This allows you to focus on complex cases and deliver better patient care.
How does AI ensure data privacy in medical imaging?
AI uses techniques like differential privacy and data encryption to protect sensitive patient information. These methods allow you to train AI models without compromising data security, ensuring compliance with privacy regulations while maintaining diagnostic accuracy.
Are AI tools in medical imaging reliable?
Yes, AI tools undergo rigorous testing and validation before clinical use. They are trained on large datasets to ensure accuracy and reliability. However, you should always use AI as a supportive tool alongside your clinical judgment.
How can AI improve access to healthcare in underserved areas?
AI-powered teleradiology and portable imaging devices enable remote diagnosis and care. These tools help you provide timely medical imaging services to patients in rural or underserved regions, bridging gaps in healthcare access.
