AI in healthcare is transforming patient care by achieving diagnostic accuracy rates of up to 99.5% in cancer detection and reducing drug production costs by billions.
|
Application |
Impact |
|---|---|
|
Personalized Treatment |
|
|
Virtual Consultations |
30% increase in access |
|
Diagnostic Tools |
Outperform human experts in speed, accuracy |
|
Cost Reductions |
Understanding both the benefits and the challenges remains essential. How does this technology reshape diagnosis and treatment today?
Key Takeaways
-
AI helps healthcare by making diagnoses more correct. It also makes treatment plans fit each patient better. This helps doctors find diseases sooner. It lets them choose the best therapy for each person.
-
AI makes healthcare work faster by doing simple jobs automatically. It helps stop mistakes and speeds up work. This gives doctors more time to care for patients. It also helps patients get better results.
-
Even with these good things, AI in healthcare has problems. It must keep patient information safe. It should not be unfair or biased. It also needs to work well with old systems. Doctors and tech workers must work together to fix these issues.
AI in Healthcare
What Is AI?
AI in healthcare refers to the use of computer systems that mimic human intelligence to support medical tasks. These systems recognize patterns, learn from data, and make predictions. Experts define AI in healthcare as a branch of computer science that uses machine learning and deep learning to improve diagnosis, treatment, and patient care. Hospitals use AI to analyze medical images, assist in surgery, and manage patient records. AI also helps doctors make better decisions by providing real-time insights.
Medical AI research has grown rapidly, with publications rising from just 15 in 1995 to over 5,000 by 2023. This growth shows strong interest and investment in the field. In the United States, about 18.7% of hospitals had adopted at least one form of AI by 2022. Adoption rates are higher in teaching and larger hospitals, while budget and policy differences affect how quickly hospitals use these tools.
Key Technologies
Several key technologies drive AI in healthcare:
-
Machine Learning: Algorithms learn from large datasets to predict diseases or suggest treatments.
-
Deep Learning: Advanced neural networks analyze complex data, such as medical images, to detect patterns that humans might miss.
-
Data Analytics: AI processes real-world data from electronic health records, wearables, and clinical notes to provide actionable insights.
|
Technology |
Example Use Case |
|---|---|
|
Machine Learning |
Predicting patient risk |
|
Deep Learning |
Analyzing X-rays and MRIs |
|
Data Analytics |
Monitoring patient health in real time |
AI in healthcare integrates with clinical practice by automating routine tasks, supporting decision-making, and personalizing patient care. Hospitals use AI to optimize workflows, recruit for clinical trials, and improve patient outcomes. These technologies help doctors deliver faster, more accurate, and more personalized care.
Diagnostics
Medical Imaging
AI-driven medical imaging has transformed the way clinicians detect and diagnose diseases. Advanced algorithms, such as convolutional neural networks, analyze X-rays, CT scans, and MRIs with remarkable precision. These systems identify subtle abnormalities that may escape even experienced radiologists. Recent clinical validation studies highlight the impact of AI in medical imaging:
|
Metric / Outcome |
Result / Value |
Statistical Significance / Notes |
|---|---|---|
|
5 studies |
Published between 2022 and 2024 |
|
|
Total participants |
929 participants |
464 in AI group, 465 in control group |
|
Improvement in image quality |
Mean difference 0.70 |
95% CI 0.43-0.96; P < .001 (statistically significant) |
|
Efficiency in image analysis |
Odds ratio 1.57 |
95% CI 1.08-2.27; P = .02 (statistically significant) |
|
Diagnostic accuracy in intracranial aneurysm detection |
High accuracy and sensitivity reported |
Specific study by Hu et al. |
|
Noninferiority of low-dose CT with AI reconstruction for liver lesion detection |
Demonstrated noninferiority |
Specific study by Lee et al. |
AI in healthcare imaging reduces human error caused by fatigue or oversight. It automates routine tasks, shortens reporting times, and prioritizes urgent cases. For example, AI models have shown high accuracy and sensitivity in detecting intracranial aneurysms and liver lesions, supporting clinicians in making faster, more reliable decisions. However, some studies note that AI works best as a complementary tool, with human oversight remaining essential.
Note: AI performance may vary depending on the imaging modality, clinical application, and real-world conditions. Ongoing research aims to improve reproducibility and integration into clinical workflows.
Early Detection
Early disease detection saves lives and improves patient outcomes. AI models excel at identifying diseases at their earliest stages, often before symptoms appear. In breast cancer screening, AI-assisted mammography increases detection rates and reduces false negatives, especially for women with dense breast tissue. These systems match or exceed the sensitivity of expert radiologists. In lung cancer screening, AI models have matched or surpassed expert accuracy in finding early-stage malignancies. Colorectal cancer screening also benefits, with AI increasing adenoma detection rates during colonoscopy, which links to lower mortality.
AI expands access to quality screening in underserved areas. Non-specialists can use AI tools to perform and interpret tests accurately, promoting health equity. By analyzing millions of patient records, AI models predict cancer risk more accurately than traditional genetic tests. They identify early disease indicators not directly linked to the affected organ, as seen in pancreatic cancer prediction studies. AI also detects cancer cells invisible to the human eye and flags suspicious areas in imaging scans, reducing the need for invasive procedures and speeding up diagnosis.
Tip: AI enhances early cancer detection by analyzing large, diverse healthcare datasets, finding subtle patterns and risk factors missed by traditional methods. This approach supports personalized risk assessment and helps optimize screening programs.
Data Analysis
AI in healthcare leverages powerful data analysis to improve early disease detection and risk prediction. Machine learning models process vast amounts of data from electronic health records, lab results, and imaging studies. These systems identify patterns that signal disease risk or progression, often before clinical symptoms develop.
|
AI Application Area |
Metric Description |
Quantitative Result |
|---|---|---|
|
Early Disease Detection (Multiple domains) |
Accuracy of AI algorithms |
|
|
ECG Screening for Ventricular Dysfunction |
Improvement in first-time detection vs. standard care |
32% increase (AUC = 0.92) |
|
Cardiovascular Risk Prediction |
Pooled AUC of ML models vs. traditional risk scores |
ML: 0.865 & 0.847 vs. Traditional: 0.765 |
|
Cardiac Ultrasound Video Analysis |
Identification of high-risk patients vs. clinical experts |
Higher accuracy than experts |
|
Large Cohort Predictive Models |
Predictive ability for adverse cardiac events |
Developed from 512,764 patients |
In lung cancer diagnosis, AI models achieve sensitivity and specificity rates as high as 0.87, with accuracy ranging from 77.8% to 100%. Machine learning models using electronic health records predict lung cancer within one year with an AUC of 0.881. Deep learning models also predict cancer progression and treatment needs with high accuracy.
Unordered list of key findings from recent studies:
-
Systematic reviews show AI reduces incorrect positive and negative diagnostic results.
-
AI improves diagnostic accuracy, especially for less experienced staff.
-
AI enhances reporting times and workflow efficiency.
-
Some studies highlight risks, such as overcalling negative findings, and emphasize the need for human oversight.
-
Larger, multicenter studies are needed to assess long-term impacts and clinical utility.
AI in healthcare diagnostics continues to evolve, offering clinicians powerful tools for early detection, risk prediction, and improved patient care.
Treatment Planning

Personalization
AI transforms treatment planning by enabling highly personalized care. Algorithms analyze genetic, lifestyle, environmental, and clinical data to tailor therapies for each patient. Reinforcement learning optimizes treatment strategies through iterative decision-making. Natural Language Processing (NLP) models, such as GatorTron, process unstructured clinical notes to support individualized interventions. Deep learning architectures, including convolutional and recurrent neural networks, interpret imaging and physiological data to predict outcomes and refine diagnoses.
Clinical collaborations, like those between Mayo Clinic and IBM Watson Health, use AI to examine genetic profiles and treatment histories. These partnerships generate recommendations that match patient needs. Platforms such as CURATE.AI adjust chemotherapy dosing in real time, improving response rates and reducing side effects. Wearable devices combined with AI enable continuous monitoring, allowing clinicians to make dynamic adjustments based on patient data.
Research demonstrates the impact of these approaches. AI algorithms optimize chemotherapy dosing by learning from patient responses, which improves efficacy and minimizes adverse effects. Predictive models forecast immunotherapy responses in melanoma patients with statistical accuracy. AI models analyzing longitudinal CT scans predict sensitivity to cancer therapies, enabling dynamic treatment adjustments. A case study from Dana-Farber Cancer Institute showed IBM Watson for Oncology achieved a 90% concordance rate with tumor board recommendations for breast cancer, reducing planning time from up to 20 minutes to just 40 seconds.
AI in healthcare personalizes treatment by integrating multi-omics data, predicting drug responses, and generating follow-up care plans based on recovery progress.
Predictive Models
Predictive models play a crucial role in anticipating patient responses and guiding therapy choices. These models use machine learning to analyze electronic health records, lab results, imaging, and wearable device data. They forecast disease progression, treatment responses, and potential complications. For example, IBM Watson for Oncology analyzes genetic data and treatment history to recommend personalized cancer therapies. Google DeepMind’s tools identify risks such as acute kidney injury before symptoms appear, allowing earlier intervention.
Predictive analytics optimize treatment plans by evaluating patient characteristics and past responses. Clinical decision support systems, like those from Epic Systems, alert clinicians to drug interactions in real time. The NIH’s All of Us Research Program leverages predictive analytics to develop personalized treatment plans from diverse health data.
The following table highlights quantitative assessments supporting the reduction of trial-and-error in cancer treatment through AI-driven predictive models:
|
Study / Model Description |
Quantitative Metric |
Value |
Impact on Trial-and-Error Reduction |
|---|---|---|---|
|
AI model predicting complete response in LARC patients (MRI texture analysis) |
AUC for complete response prediction |
0.86 |
Enables early and accurate prediction of treatment response, reducing unnecessary treatment trials |
|
AI model predicting non-responders in LARC patients |
AUC for non-response prediction |
0.83 |
Helps avoid ineffective treatments by identifying non-responders early |
|
Watson for Oncology (WFO) vs Multidisciplinary Teams in colorectal cancer |
Concordance rate |
91% |
High agreement supports AI-assisted treatment decisions, minimizing trial-and-error |
|
AI prognostic models for metastatic colorectal cancer (mCRC) therapy response |
Accuracy in distinguishing responders/non-responders |
Up to 99-100% |
Enables personalized treatment plans, reducing ineffective therapies |
|
AI classifier predicting drug resistance combining biomarkers |
AUC |
0.93 |
Improves prediction of resistance, guiding better drug selection |
|
AI models predicting compound activity against cancer cells |
AUC, Sensitivity, Specificity |
0.94, 87%, 87% respectively |
Enhances drug screening efficiency, reducing trial-and-error in drug discovery |
|
IBM Watson genome analysis time vs human experts |
Time to propose treatment plan |
10 minutes vs 160 hours |
Dramatically accelerates treatment planning, reducing delays and iterative testing |
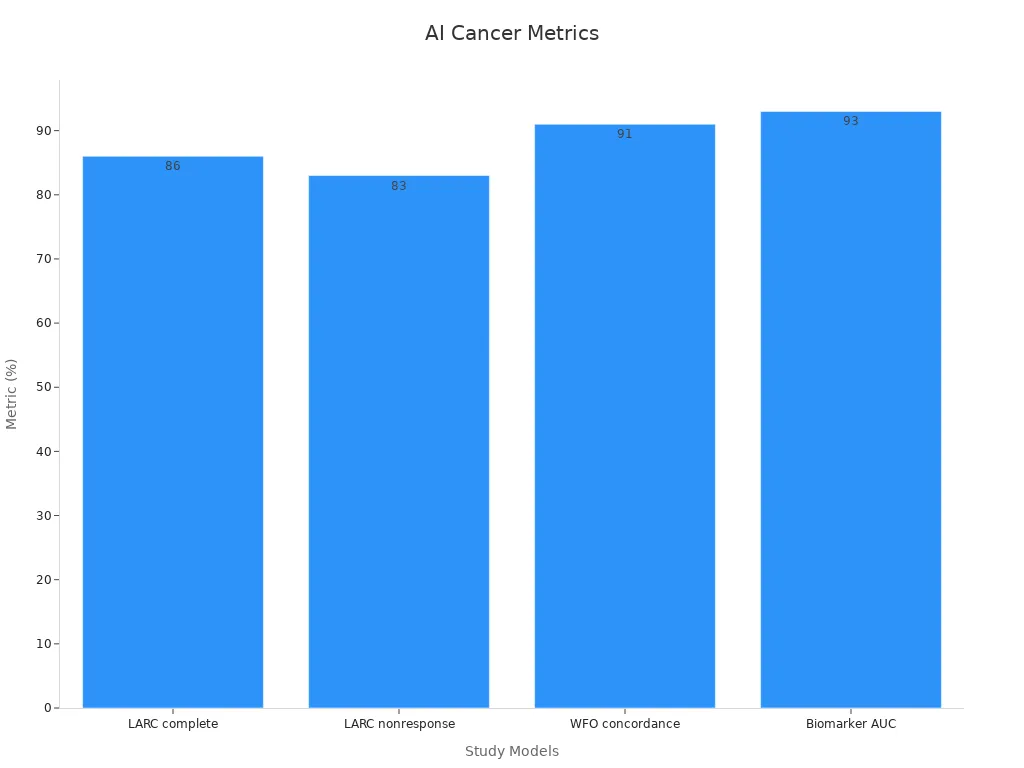
These results show that predictive models provide high accuracy and efficiency in forecasting treatment responses, drug resistance, and therapy outcomes. This supports a significant reduction in the traditional trial-and-error approach, especially in cancer care.
Decision Support
AI-driven clinical decision support systems (AI-CDSS) enhance diagnostic accuracy and streamline treatment planning. These systems synthesize data from electronic health records, imaging, genomics, and wearable devices to generate evidence-based recommendations. AI-CDSS assist clinicians in oncology, radiology, and chronic disease management by providing real-time alerts and clinical summaries.
OpenEvidence, an AI platform for primary care, received high ratings for clarity, relevance, and evidence-based support. It reinforced physician decisions, especially in chronic disease management. AI integration in electronic health records enables earlier interventions and proactive alerts, reducing clinician cognitive load and improving decision-making efficiency.
AI in healthcare supports clinicians by:
-
Improving diagnostic accuracy and personalized treatment planning.
-
Detecting diseases such as lung cancer from CT scans with expert-level performance.
-
Assisting in healthcare resource allocation and priority setting.
-
Reducing unnecessary tests and optimizing resource use.
-
Generating personalized treatment plans from diverse data sources.
-
Supporting transparency, explainability, and clinician control to ensure AI augments, not replaces, clinical judgment.
AI-driven decision support tools help clinicians deliver safer, more effective, and more efficient care by analyzing complex data and providing actionable insights.
Benefits
Accuracy
AI systems have raised the standard for diagnostic accuracy in medicine. Advanced algorithms analyze patient symptoms, genetics, and medical history to identify complex conditions. These tools reduce misdiagnosis and support timely treatment. AI-powered clinical decision support systems review large volumes of patient data, highlighting subtle patterns that may escape human notice. By providing evidence-based recommendations, AI helps clinicians detect errors in treatment plans or medication dosages. This approach enhances patient safety and ensures that care decisions rely on the most current information.
Efficiency
Healthcare organizations have seen significant gains in operational efficiency through AI adoption. Automation of administrative tasks, such as scheduling, documentation, and billing, allows clinicians to focus more on patient care. The following improvements highlight the impact:
-
Predictive analytics have reduced hospital readmissions by up to 50%.
-
AI-driven models have decreased unnecessary tests and procedures by about 30%.
-
Clinicians spend over four hours daily on paperwork; AI is projected to cut documentation time by half by 2027.
-
57% of physicians see reduced administrative workload as AI’s biggest opportunity.
-
Revenue cycle management automation has led to 20% greater efficiency in insurance claims and 18% fewer data-entry errors.
These changes streamline clinical workflows and reduce burnout among healthcare professionals.
Patient Outcomes
Streamlined workflows and accurate diagnostics contribute to better patient outcomes. AI optimizes resource allocation by forecasting patient flow and scheduling staff efficiently. Clinical decision support systems recommend personalized treatment plans and identify potential medical errors. By processing large amounts of data quickly, AI ensures that clinicians receive timely, relevant information. These advances help reduce medical errors, improve patient safety, and support more effective, individualized care.
Challenges
Data Privacy
AI systems in healthcare rely on vast datasets, raising concerns about patient confidentiality and consent. Unauthorized access and data breaches pose significant risks, especially in mobile and online health platforms. Patients often fear losing control over their personal information, particularly when data is shared with third parties without explicit consent. High-profile incidents, such as the misuse of Facebook data by Cambridge Analytica and the Royal Free London NHS Foundation Trust's unauthorized sharing of patient records, have heightened public skepticism. Transparent data governance and informed consent protocols are essential to build trust and facilitate AI adoption.
|
Challenge Area |
Description of Challenge |
Supporting Evidence / Examples |
|---|---|---|
|
Data Privacy |
Ensuring patient consent and confidentiality is difficult due to AI's reliance on large, diverse datasets. Risks include unauthorized data access and data hacking, especially in mobile and online health systems. Patients need clear opt-out rights and ongoing consent mechanisms. |
– Patient consent upholds autonomy; confidentiality fosters trust. |
Bias
Algorithmic bias in AI models exacerbates health disparities, particularly for underrepresented groups. Bias often stems from unrepresentative datasets and insufficient validation during development. For example, Black, Hispanic, and female patients are underrepresented in cardiac imaging datasets, leading to poorer outcomes. Only 4% of FDA-cleared AI products report patient demographics, leaving biases unchecked in later stages. Socioeconomic disparities also affect access to AI technologies, as wealthier institutions are more likely to implement advanced systems. NIH initiatives, such as AIM-AHEAD and Bridge2AI, aim to mitigate bias by promoting diversity in datasets and development teams.
Research highlights that AI-driven tools can perpetuate racial, gender, and age-related biases. Facial recognition algorithms often perform poorly for darker-skinned individuals, especially women of color, while older adults may distrust AI diagnostics. These biases underscore the need for transparent, inclusive AI systems designed to address inequities across multiple dimensions.
Integration
Integrating AI into existing healthcare systems presents technical, financial, and organizational challenges. Data standardization remains a major obstacle, as institutions use varying formats and coding systems. This complicates AI's ability to process and analyze dispersed patient data effectively. High costs for technology upgrades, data storage, and skilled personnel hinder adoption, particularly for smaller facilities. Employee resistance and fears of job obsolescence further complicate implementation.
-
AI integration introduces patient data privacy and security risks, making healthcare data attractive targets for hackers.
-
Variations in terminology and coding for medical conditions hinder AI processing.
-
Technical barriers include modifications to EHR infrastructures, which may disrupt care delivery.
-
Ongoing training and upskilling are necessary for healthcare workers to adapt to AI technologies.
Ethics
Ethical concerns surrounding AI in healthcare include fairness, transparency, and patient autonomy. Patients often express fears about AI replacing human roles, emphasizing the need for transparency and accountability. Informed consent procedures must include clear explanations of AI's role to improve patient self-efficacy. Intellectual property rights and proprietary algorithms raise questions about equitable access and trust. Bias audits, interdisciplinary collaboration, and international regulatory frameworks are critical to address these challenges.
Surveys reveal public fears about AI replacing human judgment and its economic impacts. Ethical frameworks, such as the AMA's policies and the SHIFT model, emphasize sustainability, inclusiveness, and fairness. These efforts aim to ensure AI complements human care rather than replacing it, fostering trust and acceptance among patients and providers.
Future Trends
Innovation
Ongoing innovation continues to reshape healthcare. Experts predict that by 2025, AI will move from pilot projects to routine clinical use, especially in diagnostic imaging and clinical decision support. After 2025, advanced systems will learn from real-world data and provide explainable recommendations. New imaging tools will combine MRI, CT, PET, and pathology data for more personalized treatment. Portable devices with AI will enable point-of-care diagnostics. Personalized medicine will use AI for pharmacogenomics and real-time clinical trial adjustments. Telehealth will expand with AI-powered triage bots and continuous monitoring from wearables. Regulatory frameworks are evolving to ensure transparency and safety.
-
Advanced imaging combines multiple data sources for tailored care.
-
Telehealth and remote monitoring grow with AI-driven tools.
-
Regulations adapt to support transparency and oversight.
Clinician Collaboration
Collaboration between clinicians and AI developers remains essential. Technology forecasts show that machine learning, deep learning, and natural language processing already improve diagnostic accuracy and early detection. New tools like explainable AI help clinicians interpret complex data and make informed decisions. Studies highlight that when clinicians work with AI, such as in radiology report generation, the quality of reports improves. Clinicians correct errors and ensure clinical relevance. Interdisciplinary research centers and translational roles help align AI development with clinical needs. Ongoing education and professional development prepare clinicians to use these tools effectively.
Clinician involvement ensures AI tools remain safe, relevant, and trustworthy in real-world practice.
Patient Care
AI technology continues to improve patient care delivery. Digital twins simulate patient data for personalized treatment plans. Early detection tools identify high-risk individuals for proactive care. AI accelerates drug discovery, reducing cancer drug approval times by six years and cutting manufacturing cycles by 25%. Diagnostic imaging tools achieve nearly 94% accuracy in cancer detection and reduce reporting delays by 91%. Patient engagement platforms personalize communication, improving satisfaction and adherence.
|
AI Application |
Impact on Patient Care Delivery |
Quantitative Data / Outcome |
|---|---|---|
|
AI in Diagnostic Imaging |
Improves cancer detection and early disease identification. |
Nearly 94% accuracy in cancer detection. |
|
Aidoc AI Radiology Triage |
Prioritizes critical radiology cases, reducing delays in reporting. |
91% reduction in reporting delays for critical findings. |
|
Zebra Medical Vision |
Automates imaging analysis for early detection and preventive care. |
Over 90% accuracy in identifying malignant lesions. |
|
PathAI Pathology Diagnostics |
Enhances pathology slide analysis for more accurate diagnoses. |
Improved diagnostic accuracy (no specific % given). |
|
Inferscience HCC Assistant |
Automates coding and risk adjustment, improving provider focus on patient care. |
Up to 30% improvement in coding accuracy. |
|
IBM Watson Health |
Uses AI and NLP to generate actionable patient insights, improving treatment decisions. |
Not quantified but improves care quality and compliance. |
|
Google Health AI Imaging |
Accelerates disease detection with high accuracy, enabling earlier interventions. |
Nearly 94% accuracy in cancer detection. |
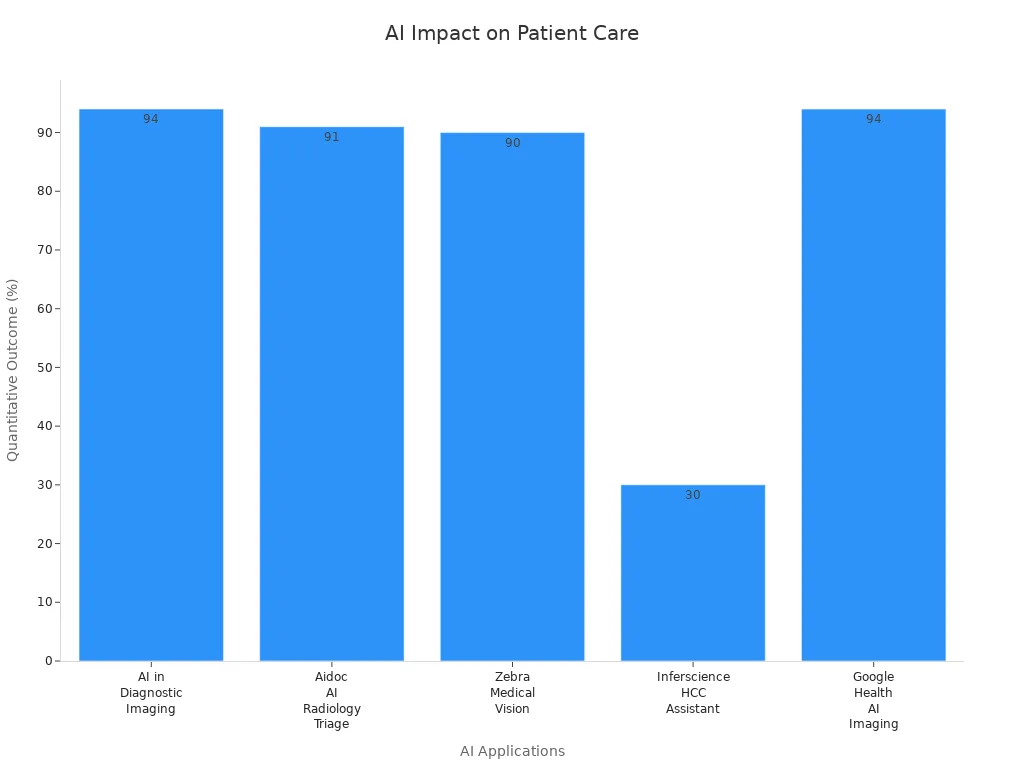
Recent studies highlight AI’s transformative role in diagnostics and treatment planning.
|
Aspect |
Result/Impact |
|---|---|
|
Health behavior change |
|
|
Hospital readmission |
Significant reduction, especially for chronic care |
|
User satisfaction |
Higher with hybrid AI-human models |
|
Key challenges |
Data privacy, trust, integration, ethics |
AI-driven tools improve outcomes, yet challenges remain. As innovation accelerates, healthcare leaders must balance opportunity with responsibility. How will society ensure ethical, equitable AI adoption for all patients?
FAQ
What types of data does AI use in healthcare?
AI uses electronic health records, medical images, genetic data, and information from wearable devices. These sources help AI systems support diagnosis and treatment planning.
Can AI replace doctors in making medical decisions?
AI supports doctors by providing insights and recommendations. Doctors remain responsible for final decisions and patient care.
How does AI protect patient privacy?
AI systems use encryption and strict access controls. Healthcare organizations follow privacy laws to keep patient information secure.
